Unveiling the Tragic Reality: The Country with the Highest Maternal Mortality Rate
Introduction
Maternal mortality, defined as the death of a woman during pregnancy, childbirth, or within 42 days after delivery, remains a grave global concern. While progress has been made in reducing maternal deaths worldwide, there are still countries facing immense challenges in this regard. In this article, we shed light on the country with the highest maternal mortality rate, exploring the factors contributing to this tragic reality and discussing potential solutions.
Understanding Maternal Mortality:
Maternal mortality is a key indicator of a nation’s healthcare system and social development. It reflects the quality of reproductive healthcare, access to skilled birth attendants, availability of emergency obstetric care, and overall women’s empowerment. High maternal mortality rates are often indicative of systemic issues and inequalities within a country.
The Country with the Highest Maternal Mortality Rate:
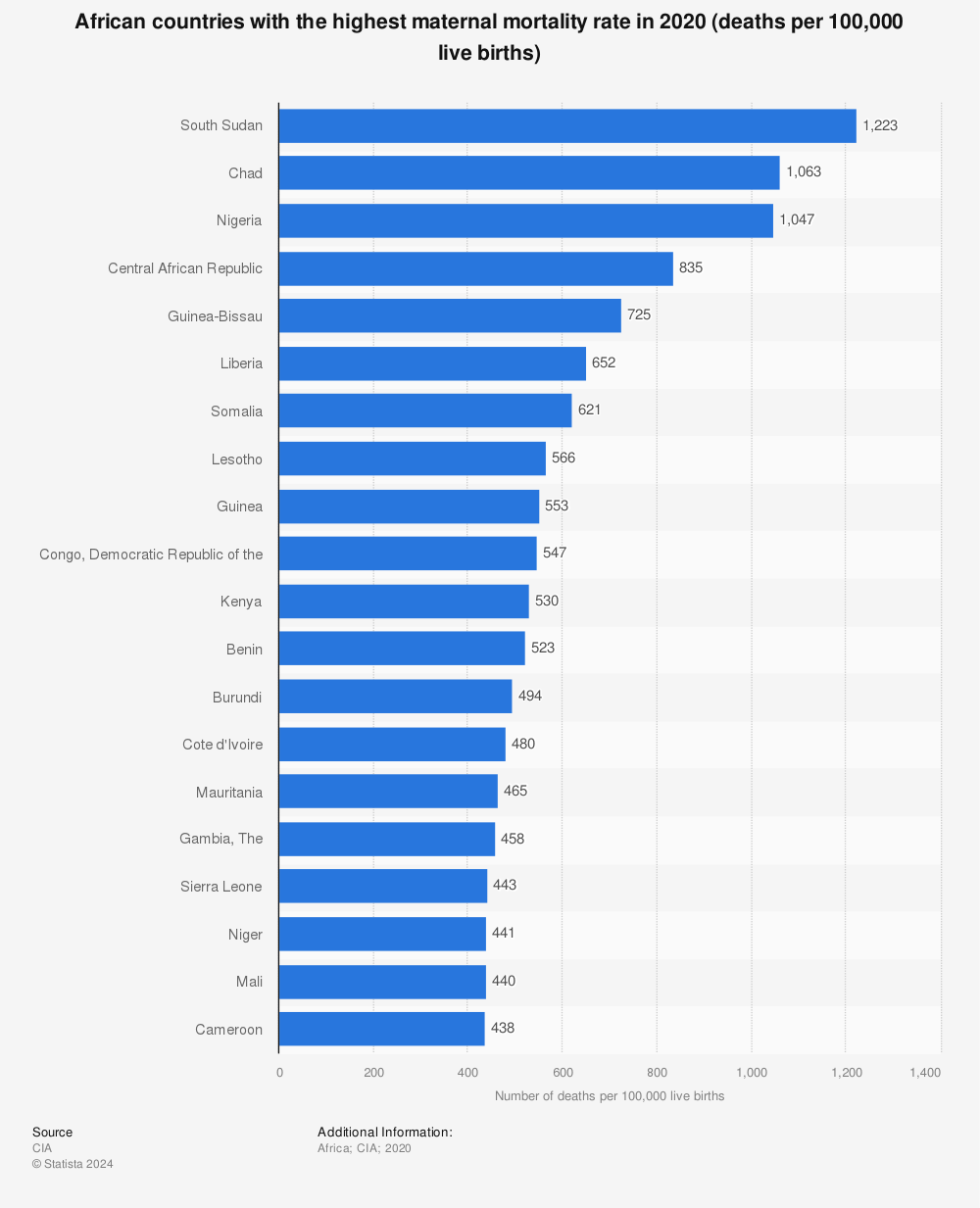
Nigeria, a populous West African nation, holds the unfortunate distinction of having the highest maternal mortality rate globally. According to estimates from the World Health Organization (WHO), Nigeria accounted for about 20% of global maternal deaths in 2017. The country’s maternal mortality ratio is estimated to be 512 deaths per 100,000 live births, a figure that is significantly higher than the global average of 211 deaths per 100,000 live births.
Factors Contributing to the Tragic Reality:
- Inadequate Access to Healthcare: Nigeria faces significant challenges in providing adequate healthcare access, particularly in rural areas. Limited availability of healthcare facilities, a shortage of skilled healthcare professionals, and a lack of infrastructure contribute to the difficulty women face in accessing essential reproductive healthcare services.
- Weak Health Systems: Nigeria’s healthcare system suffers from systemic weaknesses, including insufficient funding, poor coordination, and inadequate medical supplies. These factors hinder the provision of timely and effective emergency obstetric care, leading to preventable maternal deaths.
- Cultural and Societal Factors: Deep-rooted cultural and societal norms also play a role in Nigeria’s high maternal mortality rate. Early marriages, gender inequality, limited education, and harmful traditional practices, such as female genital mutilation and unskilled birth attendants, contribute to the vulnerability of pregnant women.
- Poverty and Socioeconomic Disparities: Widespread poverty and socioeconomic disparities in Nigeria exacerbate the challenges faced by pregnant women. Poverty limits access to quality healthcare, nutrition, and sanitation, increasing the risk of maternal complications and mortality.
Potential Solutions and Interventions:
- Strengthening Healthcare Infrastructure: Investments in healthcare infrastructure, including the construction of more healthcare facilities and the provision of medical equipment, can improve access to quality maternal healthcare across the country.
- Enhancing Skilled Birth Attendance: Expanding the availability of skilled birth attendants, midwives, and obstetricians is crucial to ensuring safe deliveries and reducing maternal deaths. Investments in training programs and incentives to attract healthcare professionals to underserved areas are necessary.
- Improving Emergency Obstetric Care: Ensuring the availability of emergency obstetric care, including access to blood transfusions, cesarean sections, and postpartum care, can significantly reduce maternal mortality. Upgrading healthcare facilities and equipping them with necessary supplies and personnel is essential.
- Addressing Sociocultural Factors: Efforts to promote gender equality, education, and awareness about reproductive health can help challenge harmful cultural norms and empower women. Community engagement and involvement of local leaders and traditional birth attendants can facilitate positive change.
- Poverty Alleviation and Social Protection: Comprehensive poverty alleviation measures and social protection programs, including maternal health insurance schemes, can address socioeconomic disparities and improve access to essential healthcare services.
Conclusion
Nigeria’s high maternal mortality rate is a tragic reality that requires urgent attention and concerted efforts from the government, healthcare providers, civil society, and international partners. By addressing the factors contributing to this crisis and implementing targeted interventions, Nigeria can make significant progress in reducing maternal deaths, ensuring the well-being of its women, and promoting sustainable development. It is imperative that the global community supports Nigeria in its journey towards achieving safe and equitable maternal healthcare for all.
