Racial Disparities in Maternal Mortality: Addressing an Urgent Issue
Introduction
Maternal mortality is a critical public health concern, and unfortunately, racial disparities in maternal mortality rates persist in many countries, including the United States. This article explores the topic of racial disparities in maternal mortality, shedding light on the factors contributing to this issue and discussing potential solutions. By understanding the underlying causes and implementing targeted interventions, we can work towards reducing these disparities and ensuring equitable maternal healthcare for all women.
Understanding Maternal Mortality
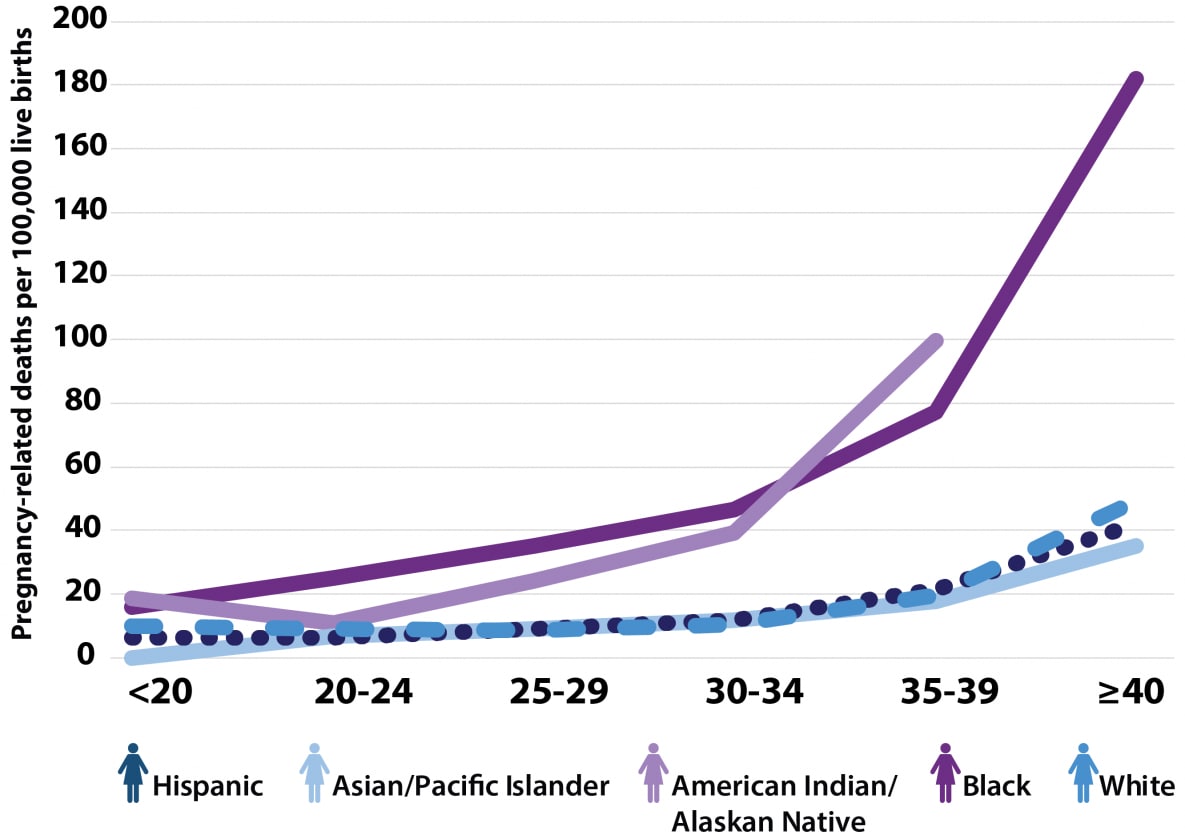
Maternal mortality refers to the death of a woman during pregnancy, childbirth, or within 42 days after delivery. Despite significant advancements in healthcare, maternal mortality rates vary widely among different racial and ethnic groups. Racial disparities in maternal mortality are evident, with women of color experiencing significantly higher rates compared to their white counterparts.
Disproportionate Impact on Minority Communities
Racial disparities in maternal mortality have long plagued minority communities, particularly African American, Native American, and Hispanic populations. Studies have consistently shown that women from these communities face a greater risk of maternal death compared to white women. These disparities exist irrespective of socioeconomic status, education, or income level.
Factors Contributing to Racial Disparities
Socioeconomic Factors
Socioeconomic factors play a significant role in maternal mortality disparities. Women from marginalized communities often face challenges related to poverty, limited access to education, and inadequate healthcare resources. These social determinants of health contribute to increased maternal risks and poorer health outcomes.
Implicit Bias and Stereotyping
Implicit bias and stereotyping within the healthcare system also contribute to racial disparities in maternal mortality. Studies have revealed that healthcare providers may hold unconscious biases that affect their decision-making and quality of care provided to minority women. These biases can lead to delayed or inadequate medical interventions, negatively impacting maternal health.
Access to Quality Healthcare
Limited access to quality healthcare services is a significant barrier for many minority women. Disparities in healthcare infrastructure, insurance coverage, and geographical barriers can impede timely access to prenatal care, emergency obstetric services, and postpartum support. The lack of comprehensive healthcare exacerbates the risk of complications and maternal mortality.
The Role of Prenatal Care
Importance of Early and Regular Prenatal Care
Early and regular prenatal care is crucial for ensuring a healthy pregnancy and reducing the risk of maternal mortality. Prenatal visits provide opportunities for healthcare providers to monitor the mother’s health, identify potential complications, and provide necessary interventions. Access to prenatal care should be a fundamental right for all pregnant women, regardless of their race or socioeconomic status.
Barriers to Accessing Prenatal Care
Several barriers hinder access to prenatal care for minority women. These include financial constraints, lack of transportation, limited availability of healthcare providers, and cultural factors. Overcoming these barriers requires comprehensive strategies such as increasing healthcare funding, expanding telehealth services, and implementing culturally sensitive care models.
The Impact of Chronic Stress
Racial Stress and Its Effects on Maternal Health
Chronic stress stemming from racial discrimination and systemic inequities has a detrimental impact on maternal health. Stress affects the body physiologically and increases the risk of developing complications during pregnancy. Minority women facing discrimination and racial stress are more likely to experience preterm labor, gestational hypertension, and other adverse outcomes.
Strategies for Reducing Stress
Reducing stress among minority women requires a multifaceted approach. Providing support systems, mental health services, and community resources can help alleviate stress. Additionally, addressing the social determinants of health, promoting social justice, and dismantling systemic racism are crucial steps towards reducing stress and improving maternal health outcomes.
Maternal Mortality and Health Disparities
Racial disparities in maternal mortality are further exacerbated by preexisting health conditions, obstetric complications, and postpartum care disparities.
Preexisting Health Conditions
Women with preexisting health conditions, such as hypertension, diabetes, or obesity, face an increased risk of complications during pregnancy. Minority women are more likely to have these underlying conditions due to health disparities and limited access to preventive care.
Obstetric Complications
Obstetric complications, including postpartum hemorrhage, preeclampsia, and cesarean section complications, contribute to maternal mortality rates. Minority women often experience delays in diagnosis and treatment of these complications, leading to worse outcomes.
Postpartum Care Disparities
Postpartum care is essential for the overall well-being of both the mother and the newborn. However, minority women often face disparities in accessing postpartum care, including follow-up visits and support services. The lack of adequate postpartum care can lead to undetected health issues and increased maternal mortality rates.
Addressing Racial Disparities
Tackling racial disparities in maternal mortality requires comprehensive interventions at various levels.
Policy Interventions
Implementing policy interventions is crucial for reducing racial disparities. Policymakers should prioritize maternal health by allocating resources, supporting community-based programs, and developing evidence-based guidelines. Policy changes can help ensure equitable access to healthcare services and improve the quality of care provided to minority women.
Community-Based Initiatives
Community-based initiatives play a pivotal role in addressing racial disparities. Engaging with community organizations, providing education and resources, and fostering trust between healthcare providers and minority communities can improve health outcomes. These initiatives should focus on culturally competent care and empowering women to advocate for their own health.
Increasing Diversity in the Healthcare Workforce
Increasing the diversity of healthcare professionals is vital for addressing racial disparities. By fostering a diverse workforce, healthcare institutions can enhance cultural understanding, improve communication, and reduce implicit biases. Efforts should be made to recruit and retain minority healthcare professionals, ensuring they have opportunities for leadership roles and influence in policymaking.
Promoting Health Equity
Culturally Competent Care
Healthcare providers should receive training in cultural competence to deliver patient-centered care. This includes understanding and respecting diverse cultural practices, beliefs, and values. Culturally competent care helps build trust, improves communication, and reduces disparities in health outcomes.
Education and Awareness
Increasing awareness about racial disparities in maternal mortality is essential for driving change. Educating both healthcare professionals and the general public about the issue can foster empathy, encourage advocacy, and promote collaborative efforts to eliminate disparities.
Collaboration and Advocacy
Addressing racial disparities in maternal mortality requires collaboration among healthcare organizations, policymakers, community leaders, and advocacy groups. By working together, we can advocate for policy changes, allocate resources, and implement evidence-based interventions that reduce disparities and improve maternal health outcomes.
Conclusion
Racial disparities in maternal mortality are a pressing issue that demands immediate attention. Through targeted interventions, including policy changes, community-based initiatives, and increased diversity in the healthcare workforce, we can strive towards reducing these disparities and ensuring equitable maternal healthcare for all women. By addressing the social determinants of health, promoting health equity, and fostering collaboration, we have the power to make a significant impact on the lives of women and their families.
Frequently Asked Questions (FAQs)
- What are the main causes of racial disparities in maternal mortality?
- Racial disparities in maternal mortality can be attributed to socioeconomic factors, implicit bias within the healthcare system, and limited access to quality healthcare services.
- How can access to prenatal care be improved for minority women?
- Improving access to prenatal care for minority women requires addressing barriers such as financial constraints, transportation issues, and cultural factors. Strategies may include increasing healthcare funding, expanding telehealth services, and implementing culturally sensitive care models.
- What role does chronic stress play in maternal health disparities?
- Chronic stress, particularly racial stress stemming from discrimination and systemic inequities, can have a detrimental impact on maternal health. It increases the risk of complications during pregnancy and adversely affects birth outcomes.
- What can be done to reduce racial disparities in postpartum care?
- Reducing racial disparities in postpartum care requires ensuring access to follow-up visits and support services. Healthcare providers and policymakers should work together to address systemic barriers, provide culturally competent care, and promote comprehensive postpartum support.
- How can individuals contribute to addressing racial disparities in maternal mortality?
- Individuals can contribute by increasing awareness about the issue, advocating for policy changes, supporting community-based initiatives, and promoting collaboration among healthcare professionals, policymakers, and advocacy groups. Everyone has a role to play in reducing racial disparities and improving maternal health outcomes.
